We begin with a comprehensive assessment of your headache problem, involving your full headache history, neurological examination and investigation as appropriate, all of which can be provided at our location, The Global Clinic, in-house. Our innovative three-tiered approach combines the following:
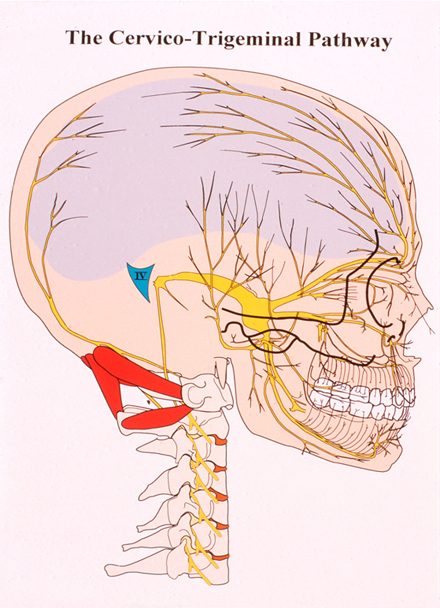
The causes of Headache have been much debated over many years. Despite the prevalence of such a common presenting symptom it is fortunate that the sinister causes of pain such as tumour and raised intracranial pressure are extremely uncommon, and of diminishing likelihood in the context of a long history of Headache without other neurological symptoms. The contribution to Headache from the Neck has a long history of enquiry, and further study exposes anatomical connections that can explain the relationship. Headache sufferers may experience a single recurring pattern of pain symptoms, but frequently suffer from more than one sort of Headache. Each Headache, e.g. Migraine or Tension Headache etc., will have a recognised time frame, distribution, and set of secondary symptoms. The pain distribution in Headache is not random. Localised pain, e.g. in the temple, above the eye, or in the cheek, occupies the territory of a definable branch of a nerve pathway. The nerve supply of the front of the head and face are served by the Trigeminal Nerve system, and the back of the head is served by the Greater Occipital and Lesser Occipital Nerves.
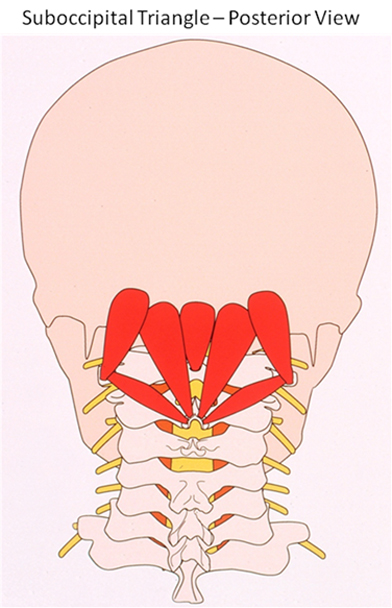
Each of these nerve systems transmits sensations from their region to the brain, but the route is not direct. The pathway involves a relay stage chain in the upper neck, called the Spinal Trigeminal Nuclei. Current Thought: In respect of muscle dynamics, which are a special interest to this clinic, recent research has highlighted potential benefits from Botox treatment in a specially-selected group of patients with Chronic Migraine. The way in which this benefit occurs is not fully agreed /still under debate, but the function of Botox in its other applications has largely been directed at counteracting muscle spasm (although it also has established benefits in managing Autonomic nerve problems). There is an implicit link that Autonomic mechanisms are involved in the maintenance of Neuropathic pain. Whilst there are surprisingly high responses in the placebo group in the major study, Botox benefits show through over 6-12 months of repeated treatments. Greater Occipital Nerve Block has been quite widely practised for a number of years, and currently finds favour in the management of Cluster Headache in leading headache centres. The way in which this helps is not proven; and unfortunately its effects have not been shown to be sustained in a number of studies. However, it is inevitable in applying this technique (though it is perceived as a Nerve block) that a key muscle attachment in the neck is also being treated: a muscle attachment that benefits the mechanisms affecting the Trigeminal Nuclei. The Norfolk Migraine Clinic: In our clinic, an extended systematic treatment of the relevant muscles has been found to potentially promote much longer-term benefits as dysfunctional Cervical muscles are rehabilitated as a set. In Headache patients, pain and spasm maintain each other in these muscles. By interrupting this vicious cycle, chronically damaged muscles regain normal function and capacity, which are sustained by an individual programme of posture and exercises. This muscle group rehabilitation leads to relief of the background stress which provokes the Nuclei which generate Migraine. Although the final common pathway of pain arises at the 1st Cervical Vertebra, contributory factors from shoulder and upper back muscles, and sources of pain generation from the lower back, must also be addressed. Principal muscles affecting the Cervical Nuclear levels are those of the Suboccipital Triangle. These interconnect the 1st and 2nd vertebrae and the major common muscle attachment at the Occiput. There are a number of defined muscles that can influence this region, producing a critical stress of this important chain of nuclei, resulting in the brain perceiving a sensation of pain at the front or at the back of the head. These muscles may become over-reactive because of a variety of preceding conditions, usually involving trauma (e.g. falls, whiplash, etc), or microtrauma in relation to postural problems.
Pain Management strategies in recent years have relied significantly on finding sources or pathways of pain, with a view to focal reduction of the inflammation or sensitivity of those sites. The first line intervention is through infiltrating an injection of anti-inflammatory steroid, usually mixed with local anaesthetic. This reduces pain activity and spasm in joints or muscles, downregulating their receptors, but causing no persisting nerve deficit. Second line treatment such as Radiofrequency Lesion applications aim to achieve persistent pain reduction by heat damage to sensitive structures. Further techniques such as surgical or chemical ablation, of nerves or other structures, are more radical. Yet more modern options involve implanted Nerve Stimulators, of considerable sophistication, - and expense. In the Norfolk Migraine Clinic, we have evolved our techniques to use muscle endplate injections of steroid and local anaesthetic, which initially numb the pain, and then provide an anti-inflammatory effect for several weeks. This cycle-breaking intervention reduces muscle inhibition and allows function to be regained through an exercise programme. The range of neck movement improves, and provocative movements become comfortable. Migraine and Headache diminish. The amount of treatment required varies from one patient to another according to extent, severity, and duration of symptoms. Most patients need two treatment sessions 8-12 weeks apart, though some more, but some only one. The aims of our therapy are to achieve significant reduction of frequency and severity of pain, a diminished need for painkillers, and a better response when they are deployed. At best, complete and enduring abolition of the presenting Headache or Migraine is achievable. For your personal treatment plan, please book an appointment on 01603 81 22 66.
|
|||||||